Mental Health & Menopause
The effects of hormonal fluctuation on the brain and body are familiar to most of us who have had regular—or irregular—menstrual cycles throughout our lives. According to both the Mayo Clinic in the US and the NHS (National Health Service) in the UK premenstrual syndrome (PMS) is a cluster of physical, mental, and emotional symptoms that a large percentage of women experience in the run-up to menstrual bleeding each month. These symptoms can include breast tenderness, bloating, headaches, fatigue, food cravings, as well as the often derided and caricatured mood swings that may have us ricocheting from crying jags to angry outbursts to doubting every choice we’ve ever made and everything we’re doing with our lives now.
In premenstrual dysmorphic disorder (PMDD) these same symptoms become severe enough to interfere with a person’s daily functioning, their ability to work, relate, and cope. According to the International Association of Premenstrual Disorders (IAPMD), PMDD affects about 5.5% of women and those who were assigned female at birth (https://iapmd.org/facts-and-figures). It is thought that those who experience PMDD have heightened sensitivity to vacillating hormone levels and respond more significantly to how estrogen and progesterone interact with various neurotransmitters.
Postpartum depression (PPD) is another manifestation of how a person can respond to plummeting levels of estrogen and progesterone, in this case the rapid drop that takes place in the first 24 hours after the birth of a baby. Because PPD is under-reported and it is estimated that up to 50% of women who experience postnatal depression will never be diagnosed, it can be difficult to know how many women are affected by it. Currently, it is estimated that 10-20% of new mothers in the US suffer from clinical postpartum depression.
For more information and statistics on PPD from different countries, broken down by race, and with regard to men see:

Both PMS and PMDD tend to vary in intensity and frequency throughout an individual’s life, sometimes not starting for years after menarche and sometimes diminishing as one matures, or emotions and life circumstances stabilize for a while. Many factors can influence the expression of PMS and PMDD including what are often called “lifestyle factors,” but—from another perspective—can also be thought of as “social determinants of health (SDOH).”

“Lifestyle” factors or Social Determinants of Health?
Lifestyle factors include things that support our well-being
· regular exercise
· eating nutritious foods
· quality sleep
· social engagement and supportive relationships
· regular visits to healthcare professionals (including acupuncturists, massage or physical therapists, etc.) to repair injury, stay current with how we’re doing physiologically, and discuss options in care
as well as things that undermine our well-being
· smoking
· drinking alcohol on a regular basis
· leading a more isolated or sedentary life
· avoiding healthcare professionals
· burning the candle at both ends
What is important to note here is that what are called “social determinants of health” have a profound impact on ACCESS to the lifestyle factors that promote well-being as well as one’s vulnerability to those factors that undermine well-being.
Social determinants of health include:
· Economic stability and access to job opportunities and income
· Educational access
· Access to quality healthcare
· One’s neighborhood and environment including exposure to pollution or toxins; access to clean water and air; safety; availability of outdoor spaces for exercise and recreation; nutritious, affordable food sources, etc.
· Social and community context—How much do people intermingle and connect? Is there a supportive and shared understanding of interdependence? Is the culture overtly or subtly racist, sexist, discriminatory, and/or violent and non-inclusive?
See Healthy People 2030 for more information on SDOH:

A woman or person’s experience of major and cyclic life events such as menstruation, pregnancy, and menopause will be significantly impacted by their environment and the level of access they have to resources that can be helpful to them.
Apart from issues with access to resources, their experience will also be heavily influenced by their perceptions about their status and identity within the cultural milieu and how this affects their stress levels and states of mind. When any one of us feels overpowered by life events or beaten down by circumstances, we are more prone to neglect exercise, eating well, or interacting with others and are more likely to sleep poorly, engage in addictive behavior, and have more negative social interactions.
This reality has an immense bearing on physical and mental well-being and is critical to keep in mind as we think and talk about menopause for all people.
My experience

It’s true that the emotional and physical symptoms associated with erratic hormones can be alleviated in menstruation, attenuated postnatally, and mitigated in menopause by doing what we can to help ourselves with food, movement, and support of various kinds.
However, it is important to recognize that during these times in our lives our internal landscapes can be so thoroughly and abruptly ransacked by hormonal changes that attempting to eat well, sleep more, and locate educated and empathic healthcare professionals can feel like swimming through a tsunami. We are working as hard as we’ve ever worked, kicking for the surface while trying to hold on to everything we’ve always done and everyone we’ve always done for, but we’re drowning. We know how to swim, and we thought we knew the currents, but this sea is shifting, becoming turbulent and unpredictable, snapping a lifetime of coping mechanisms in half and sending them to the deeps.
Melodramatic? Maybe, but this is how it has felt to me until quite recently. Clearly, not everyone will experience menopause in this way. Many people have mild premenstrual symptoms, and a large percentage of new mothers will never experience postpartum depression. Some people though are genetically or psychologically primed to be more sensitive to internal chemical shifts that profoundly impact mental and emotional health.
Most researchers agree that if you are an individual who has experienced previous bouts of depression or anxiety, events that have been traumatizing for you, or other diagnosed mental illness, you are more likely to have mental health challenges as you negotiate the menopause transition. And, if you are exposed to the added stress of being in a vulnerable position with regard to multiple social determinants of health, the situation can be exacerbated further.
If you have read the blog post on estrogen, you know that almost every cell in the body has estrogen receptors. When estrogen fluctuates and then declines during the menopause transition it effects changes in our entire limbic system, the part of our bodies responsible for managing emotions, behaviors, and memories, as well as heart rate and blood pressure. The four primary parts of the limbic system include:
· hippocampus (the seat of our memories, including traumatic ones)
· amygdala (helps to regulate emotions and stress response)
· hypothalamus (the organ that regulates not only our temperature, but sexual arousal, hunger, thirst, sleep and mood)
· thalamus (responsible for processing sensory information, memory, and emotions)
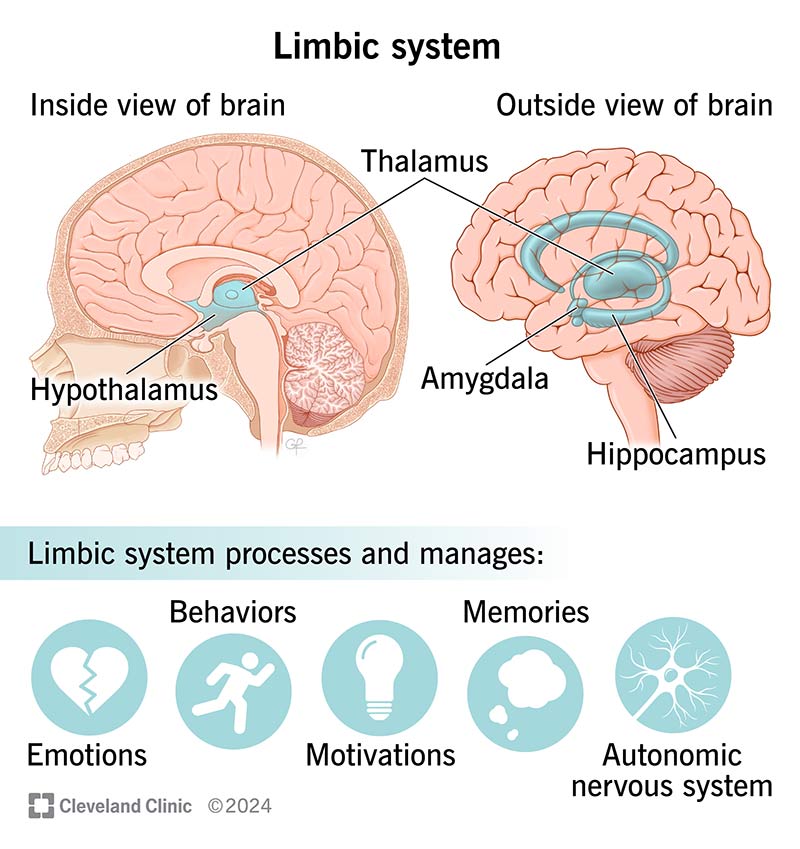
Clearly, it makes sense that we could experience moderate to severe mood swings, including anxiety, panic, or depression purely from a lack of estrogen to the cells. However, these states of mind and body might be triggered—and definitely are exacerbated by—hot flashes, insomnia, erratic eating patterns and food choices, intrusive memories, and sympathetic nervous arousal that also tend to arise because of hormonal drops.
This is what happened to me. One of the first symptoms of perimenopause that I experienced was panic attacks, usually as I was trying to fall asleep, and an uptick in anxiety and fear. This state of mind transformed my focus and energy into agitation and irritability on a consistent basis. Even so, for almost three years, distracted by the COVID pandemic, demands of graduate school, and a move across the country, I managed to negotiate (somewhat poorly, but determinedly) the agitating, undermining, disruptive symptoms of perimenopause I was experiencing. However, in the aftermath of my father’s death and my subsequent graduation in 2023, things deteriorated for me mentally and emotionally.
Starting in 2024, it felt as if I began to dissolve a little bit, my edges becoming ragged, my identity becoming increasingly insubstantial. This sensation was aggravated by a demeaning and dehumanizing job search that involved spending hours “tailoring” a resumé and cover letter to each individual job description and tossing them into the cybersphere, rarely receiving anything in response except a formulaic email assuring me that they would get in touch with me if they were interested and I shouldn’t bother them. As months passed, I began to suspect that ageism was a key factor in my inability to garner more than one response in the thirty plus inquiries I sent out. (Interestingly, the one response I did get was from a department of women who represented a range of ages from early twenties to mid-sixties.)
I started to experience “meltdowns” comprised of crying jags and despairing rants railing against circumstances both personal and socio-political. I began to think about seeing a psychiatrist again.
I had seen a psychiatrist twice before in my life—once in my mid-twenties, when a love affair that never quite got off the ground ended, and once in my early forties when I had just quit a graduate program and was going through somatic upheaval catalyzed by what was ultimately diagnosed as Hashimoto’s, an autoimmune illness affecting the thyroid gland (another producer of hormones critical to mental and physical functioning).
The first time, we experimented with anti-depressants, but categorically they didn’t work—either not making a dent in my mood or laying me out in a catatonic stupor. Finally, the doctor said, “Basically, you seem to have what I would call a combination of ‘depression’ and ‘agitated depression,’” which summed it up admirably in my view. Mood stabilizers, in this case a small dose of lithium, worked like a charm. After three years my life circumstances had changed, and with a daily yoga practice and a new career teaching yoga stabilizing me, I was able to titrate off the lithium.
The second time I saw a psychiatrist I was in Sacramento. Although yoga was still a part of my life, along with exercise, good eating habits, friends, and opportunity, nothing external to me could prevail in holding me steady when internally I seemed to be sliding apart.
When I described to the doctor what was happening inside me and what my previous experience had been, she prescribed Lamictal (lamotrigine), an anti-seizure medication often used as a mood stabilizer, along with gabapentin, another drug used to treat epilepsy and nerve pain. Both drugs calm electrical activity in the brain. With the medications helping to calm my nervous system and reduce the flood of emotion I was drowning in, I was able to address the issues confronting me, make decisions, and consolidate a new direction for myself. After 3-4 years I was once again able to stop the medications and be okay with both old and new coping mechanisms supporting me.
In September/October of last year I had four weekends in a row where I would completely fall apart emotionally for at least one day. Perhaps I was too busy during the week to unravel or perhaps I needed my husband present as a sounding board. Whatever the reason, the weekend reduced me to a seething mass of rage and grief, incapable of pulling myself together, finally wearing myself into exhaustion as the evening approached—the unsteady calm in the eye of the storm, offering some relief though I knew there was more to come.
After I graduated in December 2023, I decided to put effort into finding a therapist to help me grieve my father’s death and cope with everything I was experiencing.
The summary of my search: I do understand how difficult it can be to find someone who is taking new patients, doesn’t have a waiting list, is affordable, and clicks with you. It’s like looking for a needle in a haystack.

Finally, I found someone who could get me in after only a short wait and I worked with her for 4-5 months. Although she was sympathetic, the infrequency of our appointments (because I was paying a lot for each session out of pocket) and something about our chemistry combined so that our work together was not truly helpful, and things continued to deteriorate for me.
In September 2024 I got the name of another therapist who takes my insurance. I started seeing her; this time the chemistry was right and she has been helpful to me from the beginning. She is the one who referred me to an excellent psychiatric practice when I called her one weekend, finally at the end of my rope, deciding that I couldn’t hold out. I would need to consider medication again.
Why was I trying to hold out? I have had two healing experiences with psychoactive medications prescribed by two of the smartest, most compassionate healthcare practitioners I have ever worked with in my life. And the psychiatric PA I’ve met here in Charlotte is in the same league. Why did I feel that it would be a defeat if I started taking mood stabilizers again?
I think essentially it boils down to stigma and the incessant feeling that I am somehow doing things wrong if I can’t be okay without drugs. I didn’t want to be seen—and I didn’t want to see myself—as such a hot mess that I needed to see a psychiatrist. But when the mess started to boil, I surrendered.
The fact is—and I know this and still it was difficult to overcome my reluctance to seek the help I needed—I was so swamped emotionally, and so disarranged hormonally, that I simply could not keep pulling myself to the surface without calming the electrical storms going on in my brain. Making an appointment, seeing the psychiatrist, and starting on Lamictal once again has been a linchpin not only in recovering my balance, but in healing my relationship to my menopause experience.
I suspect there has been a strong placebo effect, because I started feeling better as soon as I took the first dose. Regardless of what, exactly, has been chemically effective, since I made the decision to get the psychiatric help I needed, the hormone replacement therapy (HRT) I had been tweaking with my primary care physician has become more effective, I completed a Menopause Yoga training, started this blog, and began a year-long writing program to help me write a menopause memoir.

A word on anti-depressants and menopause
I do know that one of the reasons I was holding out on seeing a psychiatrist was because I kept thinking that the HRT would and should improve matters. Way too often perimenopausal women go to their doctor with a list of symptoms that indicate they are in the menopause transition, and they are expeditiously diagnosed “anxious” or “depressed,” prescribed anti-depressants that will do nothing for them, and sent on their way.
If you have a history of depression and have received benefit from anti-depressants in the past, taking them in perimenopause may be helpful for you. The majority of women going through menopause, however, will not receive help from anti-depressants because their brain is missing straight up estrogen and progesterone. HRT alone is often transformative for women experiencing emotional upheaval due to perimenopause.
Please keep in mind that you do not need to have a history of mental/emotional disruption to need psychiatric help to support your menopause transition. While a history increases the likelihood that you will endure more upheaval and need targeted assistance, you may be a person who finds that the extremes of your particular menopause requires extra support for your brain, body, and mind.
Also, if you are a person who is already taking hormone therapies to support gender transitioning, you may be susceptible to the vicissitudes of hormonal fluctuation during menopause in different, as-yet-under-researched-ways. As with anyone else, it’s possible that modulating the HRT is all that’s needed to stabilize mind and mood. And it’s also possible that psychiatric care and medications may optimize body chemistry.
The siloing of medical specialties is extremely detrimental for all humans, and people going through menopause—or any kind of mental health challenge—suffer particularly. Typically, primary care physicians know very little about psychoactive meds beyond what pharmacy reps may have told them. Outrageously, the majority of OB/GYNs have almost no training in administering hormone therapy or how to recognize mental health crises that may require psychiatric medications. Psychiatrists are not routinely trained in hormone therapy or how to recognize and treat perimenopausal symptoms. We may go to one doctor and they don’t even know enough to direct us to the help we truly need.
This is enraging, frustrating, and exhausting, I know. Pause to scream, cry, run around the block, or eat a slice of cake. Drop it, go to bed, pick up the thread again in the morning and keep seeking the help you need.

Estrogen and neurotransmitters
I know this post is getting long, but bear with me for just a few more paragraphs.
Serotonin
Here are some little nuggets I recently learned about the impact of estrogen on the central nervous system:
Estradiol, the dominant, anti-inflammatory form of estrogen in our bodies, has a synergistic relationship with serotonin, a neurotransmitter that primarily regulates mood, sleep, appetite, digestion, learning, and memory. (We are probably most familiar with serotonin from our exposure to marketing about SSRIs—anti-depressants that work by inhibiting serotonin reuptake in the cells allowing more serotonin to be free in the body.)
According to Rybaczyk et al. (2005), “Estrogen receptors and serotonin receptors coexist in cells in a wide variety of tissues…[and]…Both naturally-occurring and pharmacologically-induced changes in E2 [a form of estradiol] alter the concentration of serotonin through two mechanisms” (p.2). Estradiol can both increase concentrations of serotonin the bloodstream and “acts as an antagonist at the SERT [serotonin reuptake transporter], thus promoting the actions of serotonin by increasing the time that it remains available in synapses and interstitial spaces” (p.2) Basically, estradiol can help us have more serotonin available to us more of the time.
Quantities of serotonin available in the body can have a significant impact on our psychological well-being and the quality of our sleep. Also, while we think of serotonin primarily as a neurotransmitter, it is also a hormone that regulates digestion, immune system functioning, vasodilation and clotting, and uterine contraction. Ninety-nine percent of serotonin is found in tissues other than the central nervous system (Rybaczyk et al., 2005). This gives us yet another indication of how the decline of estrogen during menopause may be triggering mental and physical health issues.
https://pmc.ncbi.nlm.nih.gov/articles/PMC1327664/
Dopamine and Glutamate
Dopamine, too, is both a hormone and neurotransmitter that affects mood, memory, and physical movement. Known as an integral part of our “reward system,” dopamine has been implicated in addiction, but is also key in keeping us motivated toward healthy behaviors that have physiological payoffs.
Glutamate is an amino acid and neurotransmitter that plays a crucial role in getting messages back and forth between neurons in the brain. It is also essential for memory, cognition, and mood regulation. It’s a precursor of GABA, a neurotransmitter known to have a calming effect.
In their paper about how estradiol affects serotonin, glutamate, and dopamine, Bendis et al. (2024), have written that “evidence supports the neuroprotective role of estrogen against diseases and injuries affecting the nervous system” (p.6).
https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2024.1348551/full
Finally, one last thing:
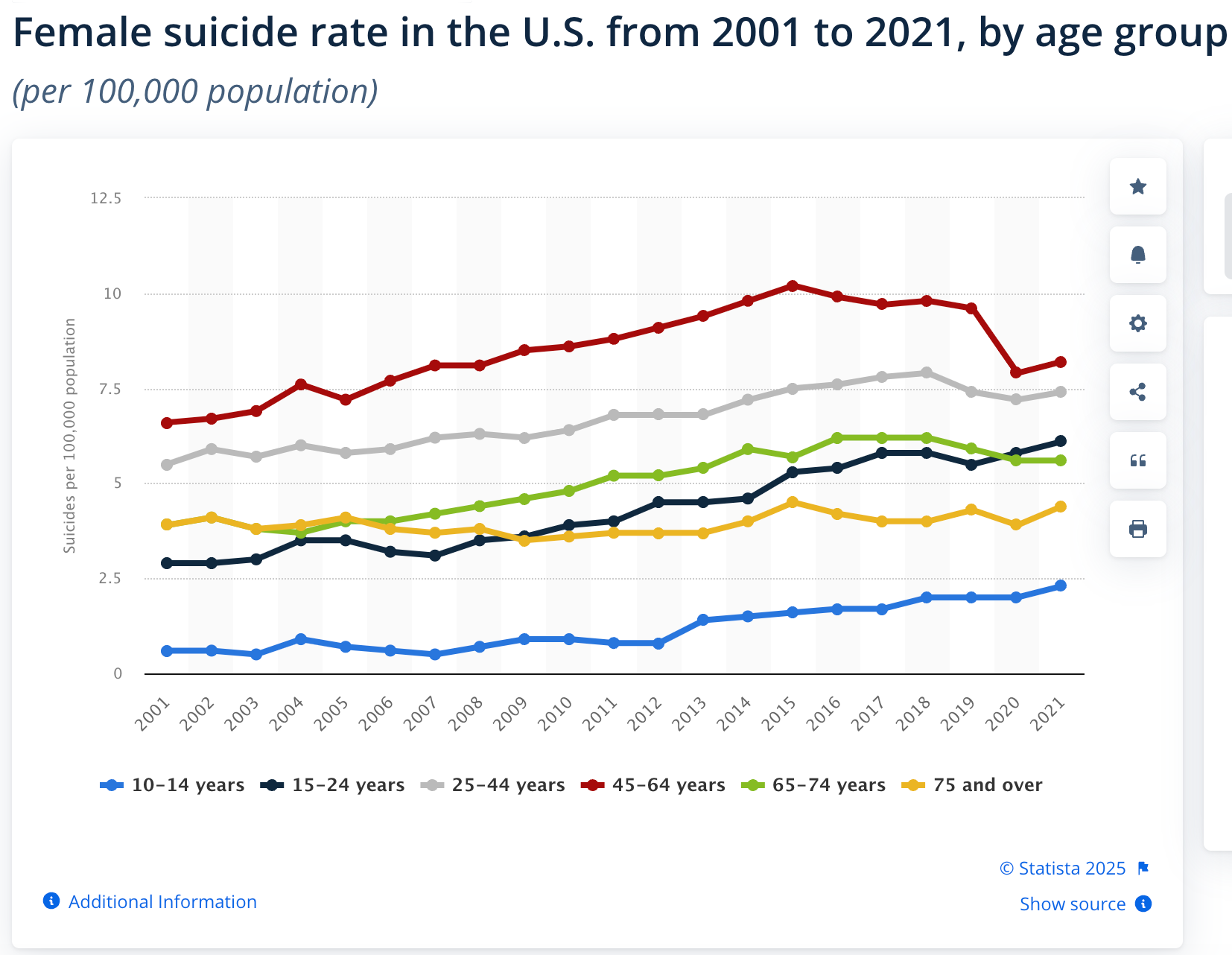
As you can see from the graph above, the rate of suicide in women is highest in the 45-64-year age group. The reasons why this is so have not been scientifically determined and are likely myriad and complex. However, clearly there is evidence to suggest that the hormonal havoc of the menopause transition coupled with the intensified stress of mid-life complexity may be challenging enough for some women to contemplate and carry out suicide.
There are a lot of elements that will determine whether or not a person chooses to take their life. Some of these factors will mitigate risk and some will increase it.
Key factors that reduce risk of suicidality:
· Access to affordable, competent physical and mental healthcare
· Access to and knowledge about nutritious food that is affordable and doesn’t take three hours to prepare
· Sleep hygiene that allows at least 7-8 hours of decent sleep per night
· Access to safe spaces for outdoor recreation
· Access to information about exercise and movement and places to do them
· Spiritual practices
· Positive, safe connections with intimate friends and family
· Feeling connected to larger community—neighbors, church, classes, groups
I know how difficult it is to search for help when you are at the end of your tether, exhausted, angry, grieving, meeting the demands of daily life while feeling that you can’t take one more step. I know how enraging it can be to pay the money, take the time, ask for help and be denied repeatedly by people who claim to be helping professionals, but are incapable of helping you.
It’s so important to keep trying. And one essential aspect of this is to keep talking to others, sharing information, making connections and building trust with people who are also walking this path of menopause, so that you can reveal what you need safely and be pointed in new, perhaps helpful, directions by others who share some of your experience.
(This week I should have time to post breath and posture practice suggestions for anxiety, depression, and balance on the "Support" page. Check them out if you're interested.)
If you would like to share your story or any resources you have found helpful in your menopause journey, please contact me at beingthechange.us@gmail.com. I will post it on the Community page.
Please include the following:
- Your question, comments, or correction
- If it is okay for me to place your question/comment/correction on the “Community” page
- What name and/or location (ex, city, state) you would like me to use to identify you


