Biology is not destiny, part 1: The Bladder

So…bladder bugaboos and pelvic organ prolapse (POP). I know it seems like the bad pelvic news keeps coming, but I wanted to address these issues after discussing GSM (genitourinary symptoms of menopause), because although there is some overlap in symptoms, GSM is typically distinct from bladder issues that can crop up during menopause in etiology (origin/cause), progression, and treatment. POP is also most productively and accurately viewed as a separate condition from GSM, though it does tend to get lumped into “conditions endemic to menopausal women.”
The first thing to keep in mind is that pelvic organ prolapses and bladder issues typically have more to do with aging than with menopause. The menopausal fluctuation and decline in both estrogen and progesterone clearly do affect tissues and blood flow in the pelvic region and it seems logical that this would contribute to prolapse and bladder sensitivities. However, in the case of POP there is currently no data that confirms the absence of estrogen as a cause of prolapse.
One 2019 study by Dietz et al. found that “duration of estrogen deprivation is not an independent predictor of PFM [pelvic floor muscle] contractility, and HRT use is unlikely to have a beneficial effect on pelvic floor muscle contractility [i.e., how efficiently and effectively the PFM contracts].”
Although there is, predictably, not a lot of research into the details of what contributes to pelvic floor muscle weakness, the general consensus at this point is that there are a few factors that exert a greater influence on the pelvic floor than the presence of specific hormones. Most of these have to do with trauma to the pelvic region and with the aging process, which, it can be helpful to keep in mind, is distinct from the menopausal process even though it is rarely treated as such.
Quality of Life
The second thing to keep in mind is that bladder and urinary issues, as well as pelvic organ prolapse issues, are not really “issues” unless they are interfering with a woman’s quality of life. Interestingly, “Although about 41% to 50% of women present with POP on physical examination, only about 3% are symptomatic” (Aboseif & Liu, 2022). Similarly, some women do not experience incontinence as something that interferes with their activities to an extent that their quality of life deteriorates. It may be infrequent, or they may find it easy to manage with straightforward fixes like over-the-counter pessaries or a sequence of daily pelvic floor physical therapy exercises.
As with so many of the changes that confront women as they negotiate the menopause transition, a patient-centered approach that takes into account how that particular person’s symptoms are manifesting and affecting her quality of life—including her work, relationships, confidence, body image, and self-esteem—is crucial.
There is an immense amount of information about pelvic organ prolapse, so in this post we will first focus on the
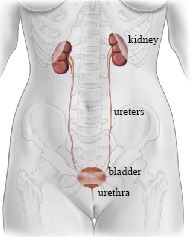
Bladder
Dr. Jen Gunter writes in her book The Menopause Manifesto, “one common theme in bladder-related concerns is their near-absence from public discourse” (p.179). She and Dr. Rena Malik, a urogynecologist who was interviewed in a podcast by Mel Robbins, both agree that while it is typical for women to develop bladder conditions as they age and hit menopause, it is not “normal,” i.e., recurrent urinary tract infections (UTIs), urinary incontinence, urgency, and frequency, and caruncles are not normal expressions of the human body as it ages. They are conditions that develop in response to invasive organisms such as bacteria or because of structural weaknesses and vulnerabilities that are not inevitable.
(There are time stamps in the episode notes to help you find information of interest.)
Yet because of embarrassment, stigma, ignorance and/or shaming on the part of healthcare professionals, women are consistently going undiagnosed and untreated with conditions that significantly impact their quality of life and which, in the majority of cases, can be successfully and non-surgically treated.
Issues that arise with the bladder may be primarily menopause related, for example, recurrent UTIs tend to be a symptom of GSM and often crop up because the lack of estrogen in the genitourinary area leads to dryness, muscle atrophy, and imbalances in the vaginal microbiome that foster an environment conducive to unfriendly and infection-causing microbes.
However, bladder problems can also be related to age, weakened muscle and fascia (connective tissue) in the pelvic area, and even behavioral habits.
UTIs
Urinary tract infections are the result of an overgrowth of bacteria in the urine that leads to inflammation and pain. The primary symptoms are pain with peeing (dysuria), needing to pee more often, and having a lot of urgency about peeing. In some cases, there is blood in the urine (hematuria).
A diagnosis of recurrent UTI happens when a person experiences:
o 2 infections in 6 months
OR
o 3 infections in 12 months
Treatment & Prevention
If you think you have a UTI, it is critical to get a urine culture and treatment. The culture will tell the doctor what kind of bacteria are present so that they can know what kind of antibiotic to prescribe to knock out the infection. Particularly if a woman has a history of taking antibiotics to treat recurrent UTIs, she may develop an infection with bacteria resistant to antibiotics she’s taken in the past.
Risks of not treating urinary tract infections include the possibility of developing kidney infections and long-term kidney damage, generalized sepsis, and death. Older women are particularly at risk of death from untreated or undertreated UTIs, either from sepsis itself or the delirium that can attend sepsis and lead to accidents and falls. Dr. Charlotte Gooding, speaking about the older women in care homes she works with, is quoted in The Guardian as saying, “Mortality in urosepsis is huge” (Muir, 2023). Qiang et al. (2016) list old age and female gender as the top risk factors for incurring urosepsis.
Typically, UTIs can be easily treated and there is a lot that can be done to help prevent them.
o Vaginal estrogen should probably be the first line of defense for peri- and post-menopausal women if it can be tolerated and a woman feels comfortable using it. Because most UTIs in aging are due to declines in estrogen levels, supplementing with estrogen can be very effective in preventing UTI. Vaginal estrogen works locally and does not seem to be absorbed into the bloodstream so there are no systemic benefits or risks. However, if a woman does not feel comfortable using estrogen, vaginal DHEA may be helpful.
o If a woman is prone to chronic urinary infection, antibiotics can be taken intermittently to prevent recurrence. Likewise, if sex seems to be the underlying trigger for UTI, antibiotics can be taken directly after sex to reduce the risk of infection.
Two other preventives mentioned by Dr. Gunter:
o Methenamine hippurate, an oral medication that converts urine to formaldehyde. This prevents bacteria from growing.
o D-Mannose, a sugar that may inhibit how bacteria bind with bladder tissue.
Dr. Gunter writes that there is very limited to no reliable data that cranberry juice, vitamin C, or probiotics are effective in preventing or treating UTIs. However, as I mentioned in the post on GSM, there have been studies that suggest there may be ways to support the vaginal microbiome either directly with probiotics administered vaginally or through the gut by supplementing orally. At this point, such a course of action is not evidence-based. However, it seems possible that some women may find probiotics effective in preventing UTIs or helping with GSM symptoms. Anecdotally, I have heard women swear by cranberry juice. Maybe the effects are due to cranberries, maybe they’re due to placebo.
The take home is to find what works for you without resorting to outright quackery or “treatments” that may hurt you and to make sure that if the UTI recurs or does not seem to be going away, get treated ASAP.

Incontinence
According to Dr. Rena Malik more than one-third of women deal with urinary leakage.
o Stress urinary incontinence (SUI): When an activity that creates or increases pressure in the abdomen leads to the leakage of urine. Coughing, laughing, sneezing, or heavy lifting can all do this.
o Overactive bladder (OAB): The bladder becomes hypersensitive and contracts to release urine even when it isn’t full. This can lead to urgency and emptying of the bladder before a person can get to the bathroom.
Rick factors for incontinence
o Aging processes that affect muscle mass, strength, and contractility
o Decline in estrogen and progesterone that affect the collagen and physiology of muscle and connective tissue
o Genetics
o Tissue damage giving birth vaginally
o Obesity
o Smoking
o Constipation, which can lead to straining in order to evacuate the bowels. This in turn can damage the tissues.
o Work involving heavy lifting and/or exercise that involves lifting but is done while holding the breath, creating pressure in the abdominal cavity.
o Neurological issues: All the functions in the pelvic region, including sexual performance and waste elimination, are intimately interconnected neurologically. An injury to the spine or a miscommunication between pelvic nerves and the brain can contribute to dysfunction in the pelvic organs/structures.
Diagnosis
Bladder function tests to determine how well the bladder is emptying or how full it is getting may be done. Imaging procedures like ultrasound or MRI may also be used.
Treatments
Wearing diapers does not need to be considered the best or only option for dealing with urinary incontinence. Most treatments for incontinence are simple and non-surgical.
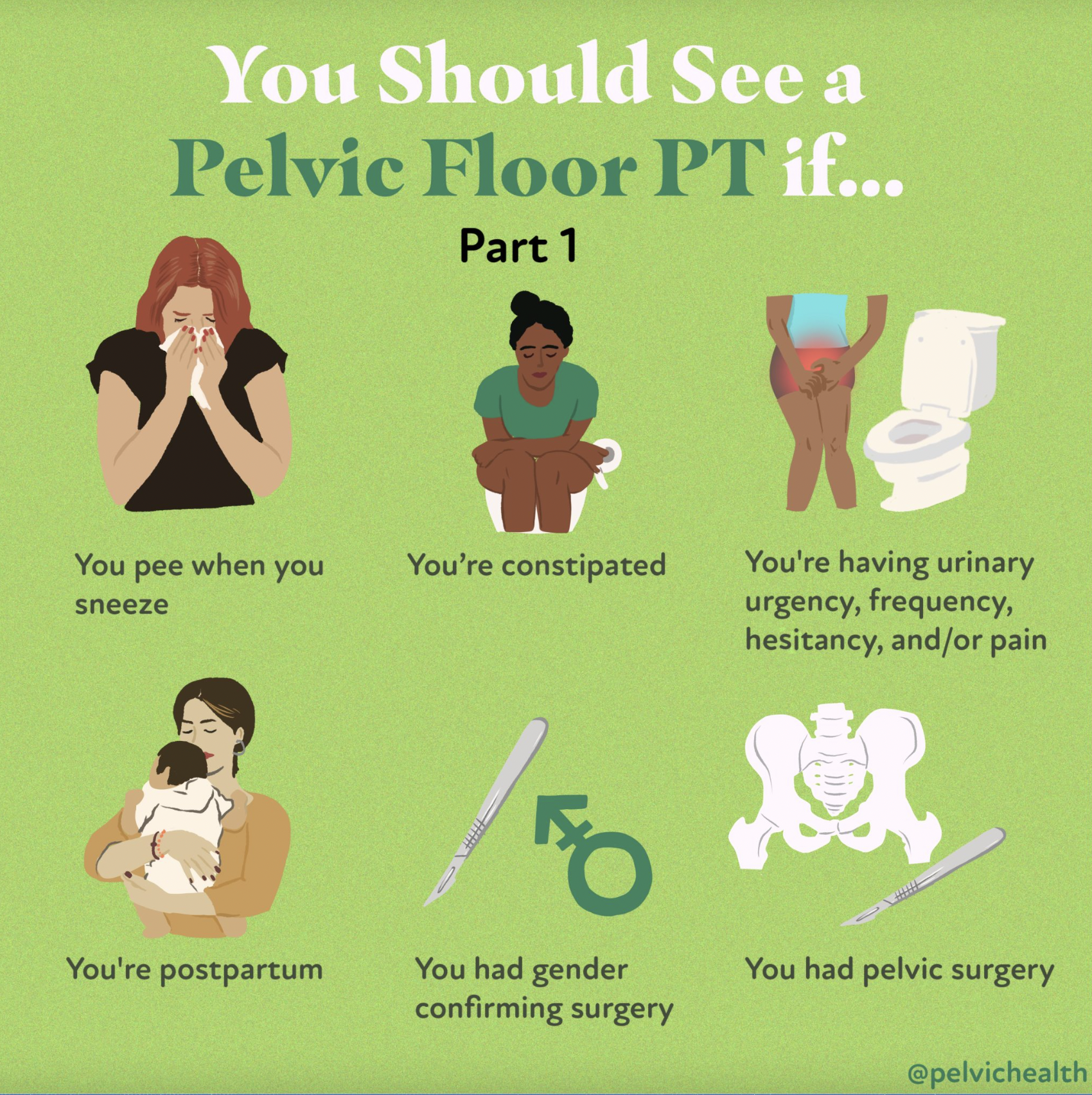
Pelvic floor physical therapy is an effective, non-invasive treatment option that is likely to have beneficial ripple effects throughout the pelvic region and body.
Pessaries, which are tampon-like devices that can be inserted into the vagina to provide support for the urethra, can be helpful, and there are a couple that are available over the counter:
o Poise Impressa:
o Uresta:

Pessaries are often used in cases of prolapse as well, to support pelvic organs when muscles and ligaments are unable to do so. However, these pessaries need to be fitted by a doctor: “Even with advanced POP, a correctly fitted pessary will be successful for approximately two-thirds of women” (Gunter, 2021).
Incontinence rings do the same job as pessaries but are reusable and can be used for longer periods of time. These will need to be fitted by a doctor.
Oral medications may be effective in reducing bladder contractions:

Vaginal estrogen can be used, but this is only likely to be helpful if the absence of estrogen in the tissues is the root cause of the incontinence symptoms. Also, as I mentioned in the GSM post, although we do not know why systemic hormone therapy can make urinary symptoms worse.
Botox injections can also be helpful for OAB, but it’s important to get as much information as possible about it. According to a patient fact sheet from the National Health Service in the UK, “Up to one in 20 women may have difficulty emptying their bladder fully after Botox treatment.” If this happens, a woman may have to self-catheterize multiple times a day until the Botox wears off.
Urethral Bulking is when a bulking agent is injected around the urethra in order to provide stability and support.
Percutaneous Tibial Nerve Stimulation (PTNS). This is a minimally invasive, fairly effective treatment based on acupuncture. It is described by Dr. Malik at about 49 minutes into the podcast with Dr. Robbins, or you can read about it here:

In some cases, surgery may be the best option for both SUI and OAB.
o For SUI a strip of mesh can be placed beneath the urethra to offer support in the same way a pessary does. This is called a midurethral sling.
o For OAB, a device that stimulates the nerve that supplies the bladder can be implanted. This is most often done once all other options have been explored and failed.
Here is a patient decision aid for SUI surgeries created by the UK’s National Institute for Care and Excellence (NICE):
Lifestyle factors
Weight loss can also be an effective way to manage or reduce incontinence. The more weight there is bearing down on the structures and muscles of the pelvic floor, the more work those muscles have to do. Dr. Malik says in the podcast that even losing 8% of one’s body weight can significantly improve urinary issues.
Smoking itself is an irritant to the bladder. Additionally, if a chronic cough is due to smoking, eliminating the source of the cough can reduce pressure on the pelvic region.
Timed voiding (urinating on a schedule) and keeping a bladder diary to track fluid intake and outgo can also be helpful for creating awareness about factors contributing to OAB and making behavioral modifications.
Some foods/drinks, in particular, caffeine, alcohol, and artificial sweeteners can irritate the bladder, and some medications may act as diuretics, increasing the volume of urine.
Caruncles
This is an awful sounding word that describes “a condition where the loss of tissue support causes cells of the urethra to protrude and become irritated” (Gunter, 2021). Although it can look scary, it’s not cancerous and tends to respond well to topical estrogen treatments.
Conclusion
What I read and heard repeatedly while researching this post is how important it is for women to understand that incontinence and pelvic floor issues are not normal, do not have to be put up with, and can often be resolved simply and effectively, vastly improving quality of life. A majority of women deal with incontinence or pelvic organ prolapse at some point in their lives and no one needs to feel as if they are strange or shameful for experiencing these things.
Urogynecologists and pelvic floor therapy specialists are the people to find for help in diagnosing and treating bladder and pelvic floor problems.
In the next post, we will explore the very common ailment of pelvic organ prolapse in some detail.
Resources
Aboseif, C., & Liu, P. (2020). Pelvic organ prolapse. https://www.ncbi.nlm.nih.gov/books/NBK563229/
Dietz, H. P., Socha, M., Atan, I. K., & Subramaniam, N. (2020). Does estrogen deprivation affect pelvic floor muscle contractility?. International urogynecology journal, 31, 191-196. https://doi.org/10.1007/s00192-019-03909-w
Gunter, Jen. (2021). The Menopause Manifesto. Citadel Press.
Muir, K. (2023, December 17). ‘Millions of women are suffering who don’t have to’: Why it’s time to end the misery of UTIs. The Guardian. https://www.theguardian.com/society/2023/dec/17/millions-of-women-are-suffering-who-dont-have-to-why-its-time-to-end-the-misery-of-utis
Qiang, X. H., Yu, T. O., Li, Y. N., & Zhou, L. X. (2016). Prognosis risk of urosepsis in critical care medicine: a prospective observational study. BioMed Research International, 2016(1), 9028924. doi: 10.1155/2016/9028924
Image References
Title image: https://www.upsondowns.co.uk/product/UD01449-toilet-womens-brite-crossed-legs-square/
“You should see…”: https://pelvicpainrehab.com/blog/6-unexpected-reasons-to-see-a-pelvic-floor-physical-therapist/



